
Hi, my name is George and I’m a second year Andrology trainee at the Shropshire and Mid Wales Fertility Centre. Andrology is a relatively new specialism so there aren’t currently many trainees or fully qualified Andrologists, and it may not be as well-known as other specialities, so hopefully I can give a bit of an insight into what the role involves!
What is Andrology?
Andrology is the branch of science relating to male reproductive health, so the clinical scientist role covers working with male patients struggling with infertility, preserving male fertility for those who may become infertile in the future, and dealing with sperm donation, which is a vital resource for those who cannot produce or use their own sperm. It is a varied role, so tasks may be different from day-to-day and different clinics may place difference emphasis on each of the areas within the field depending on their clinical workload.
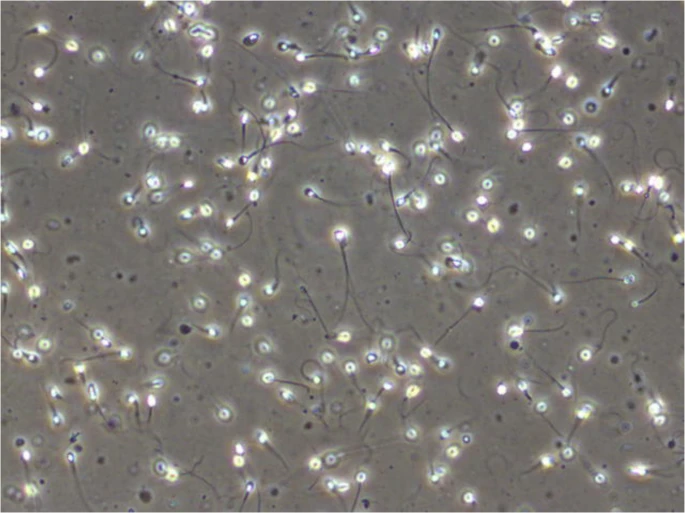
Diagnosing male infertility is a key part of the role. A diagnostic semen analysis is the primary technique used to assess a man’s fertility and is commonly performed and interpreted by an Andrologist. How many sperm cells, how they swim, and what they look like, are all analysed. If any of these are abnormal, the patient may be referred for further investigations to find possible causes, such as measuring hormone levels, a physical examination of the testes, or genetic testing. Some laboratories will perform more advanced sperm tests, such as assessing the DNA quality carried by the sperm or using computer-aided analysis to obtain more complex sperm motility data. The results of all these tests would inform the treatment plan, which could range from lifestyle advice, a referral for in-vitro fertilisation (IVF) treatment, or the use of donor sperm in cases with a very poor prognosis. A semen analysis is also performed to determine the success of a vasectomy procedure, in which there would ideally be no sperm cells present.
In terms of treatment, an Andrologist could be involved in the treatment of patients who are undergoing in-vitro fertilisation procedures (IVF), where sperm cells fertilise an egg in a dish, or those undergoing intra-uterine insemination (IUI), where sperm samples are placed into the uterus. Sperm samples used in these procedures must be prepared by separating sperm cells from semen and its constituents, and then collecting the best cells. The sample is then ready for use in IVF treatments, which will be performed by an Embryologist. Furthermore, if sperm needs to be retrieved directly from the testes, an Andrologist may be involved in searching for sperm cells in the fluid and tissue taken during a medical procedure called a surgical sperm retrieval (SSR). Any sperm found can then be used in IVF treatments.
Sperm banking is where sperm from fertile people are collected, frozen in liquid nitrogen, and can be stored for many years until the patient wishes to use them. Not only will an Andrologist perform this procedure, but they are often also involved in taking informed consent from the patient, which will include a discussion of key issues such as the length of storage and who can use the samples. Many patients who use this service are those who are about to undergo potentially sterilising medical treatment, such as cancer patients, whose treatment may involve exposure to toxic substances that may cause infertility, transgender patients, because the surgery could involve removal of the testes, and vasectomy patients, because the sperm transport tubes are to be sealed. Sperm banking therefore gives these patients the chance to have biological children in the future even if they become infertile.
The final key area of an Andrologist’s role is donor sperm. This involves recruiting donors, distributing samples to, and receiving them from, other centres, and using these samples in treatment. Donor sperm is commonly used by same sex couples, single women, or heterosexual couples where the male partner cannot produce his own sperm. Prospective donors must undergo extensive screening and must have given their informed consent once a discussion surrounding related issues has taken place. Andrologists manage this screening and recruitment process to ensure the donor samples are safe prior to use in any treatment and that they are of sufficient quality. In addition, Andrologists may match prospective patients to donors based on desired characteristics and refer them for counselling on the issues surrounding the use of donor sperm in their treatment.

Why is Andrology important?
Fertility has a significant impact on people’s lives, whether that be by having children or being unable to have children, so it is a speciality that can make a hugely positive difference to our patients. Having children is almost taken for granted by many people, yet it is not always straightforward. Approximately 1 in 10 couples struggle to conceive naturally, and in around half of these cases there is a male factor issue (Agarwal et al., 2021). This means there are so many people that may struggle to have children without the help of reproductive specialists.
Andrology in particular is important because infertility is often seen as a female problem, when male infertility may be just as common. Currently there are relatively few options for treating male infertility so patients are often referred for IVF procedures, where the female partner will undergo invasive medical procedures even if they are completely healthy. Therefore, having male fertility specialisits is vital for developing our understanding and treatment of male fertility, which should help to reduce the burden of infertility treatment on women.

Furthermore, many people undergo medical treatments which could cause them to become infertile but may still wish to have children in the future. Menawhile, those who use donor sperm often use this service as a last resort because they have no chance of conceiving naturally. The andrology services of sperm banking and donor sperm provision are therefore vital for allowing these patients the opportunity to have a family, which is hugely important to many for a range of reasons.
Why do I enjoy it?
I am fascinated by how life begins from just two tiny cells and the different factors that affect its success. This field is constantly evolving as our understanding of how sperm cells and eggs combine and interact to form a healthy baby develops. There are still so many unknowns being researched and new ideas under development, and it is exciting to me that in the future there will be new technologies introduced to improve the help we can give to patients.
I also like that there is both laboratory work and patient interaction within my role. Practical scientific processes in the lab that help people to fulfil their dreams of starting a family make up most of the work, yet there is also communication with patients, particularly regarding fertility preservation and sperm donation. These personal interactions help to reinforce that whilst what you are doing in the lab may become routine, to your patients it could make a massive difference to their lives.
George Southall-Brown, The Shropshire and Mid Wales Fertility Centre/The Shrewsbury and Telford Hospital NHS Trust
Twitter @GSouthallBrown & Instagram @georgesouthallbrown
